Hyperbaric Oxygen as an Adjuvant for Athletes
In recent years, the development of new rehabilitation techniques and regimes for sports players with injuries has advanced rapidly. The knowledge of medical doctors and trainers has grown beyond conventional Western medical treatment to also include Eastern medicine. This increased consciousness of alternative forms of treatment has positively affected the players, with an improvement in choice of rehabilitation. One such treatment that has recently captured attention is hyperbaric oxygen (HBO) treatment. Conventionally HBO has been used in medical treatments such as cerebral infarction, car- bon monoxide poisoning and the bends (decompression disease). The British physiologist Henshaw carried out the first HBO treatment using an air press organ in 1662.[1] This advancement spread to the rest of Europe in the 19th century, and to the US in the first half of the 20th century. Initially, the effective- ness of the treatment was overestimated, and it was slowly dropped by institutions and declined in popularity. It remained mostly unused until, in 1960, Boerema of the Netherlands brought it back into the spotlight. He reported that pigs, which inhaled oxygen with three times atmospheric pressure for 15 minutes, were able to survive and make a full recovery, despite having almost all erythrocytes re- moved.[2] However, widespread use of HBO in sports medicine only came about with advances in technology. The equipment that pressurises pure oxygen must have a high standard of safety, not only regarding pressurisation, but also for preventing the oxygen from igniting. HBO was first tried on a sports injury in Scotland, where it was used to treat the injuries of professional soccer and golf players in the late 1980s. James et al.[3] reported that the disease period of the damage was shortened by 70%. The interest in HBO treatment for sports injuries has since spread, especially in Japan. This article discusses the theoretical background and the clinical application of HBO to sports players.
1. The Necessity of Oxygen for Sports Players
1.1 The Effectiveness of Oxygen Against an Injury
Natural recovery works in an organised manner following a sports injury such as a fracture, ligament injury or other damage. Generally, this recovery process is classified by three phases: inflammatory, proliferative and remodelling. Oxygen plays a crucial role in each of these phases.
In the inflammatory phase, the hypoxia-induced factor-1α, which promotes, for example, the glycolytic system, vascularisation and angiogenesis has been shown to play an especially important role. However, if the oxygen supply could be controlled without promoting blood flow, the blood vessel permeability could be controlled to reduce swelling and the associated sharp pain.
In the proliferative phase, in musculoskeletal tissues (except cartilage), the oxygen supply to the damaged area is gradually raised and extracellular matrix components such as fibronectin and proteogycan are synthesised. The oxygen supply is essential for the synthesis of these extracellular compo- nents. Certain processes, such as the hydroxylation from proline to hydroxyproline, cannot be per- formed in the rough endoplasmic reticulum without oxygen, so collagen synthesis becomes impossible.
In the remodelling phase, tissue is slowly replaced over many hours using the oxygen supply provided by the blood supply vessel already built into the organisation (except cartilage) of the musculoskeletal system. Thermotherapy or massage to the damaged area can also improve oxygen circulation and improve recovery. If the damage is small, the tissue is recoverable with nearly perfect organisation. If the extent of the damage is large, a scar (consisting mainly of collagen) may replace tissue. Consequently, depending on the injury, this collagen will become deficiently hard in the case of muscle repair, or deficiently loose in the case of ligament repair.
Oxygen is generally advantageous to tissue formation and organisation, except in the case of hyaline cartilage, which needs a low oxygen environment to maintain a low frictional coefficient. It has also recently been pointed out that stem cells are involved in the recovery process. Stem cells are always being released into the blood from marrow, where they patrol the inside of the body. Mesenchymal stem cells, once gathered at the location of damage, differentiate into osteoblasts, fibroblasts, or chondrocytes according to the environment of the injury. Therefore, the role of oxygen in recovery promotion involves many factors, such as cell proliferation, differentiation and extracellular matrix production.
1.2 The Effectiveness of Oxygen Against Recovery from Fatigue
Fatigue produced by physical exertion is considered to be physiological fatigue, and is defined as ‘being in the recoverable state of a transient functional fall physiologically and mentally’, which is distinct from pathological fatigue. There are three main causes and mechanisms that result in physiological fatigue:
• diminishment of an energy source;
• accumulation of a fatigue substance; • malfunction of metabolism regulation.
The human body is continuously maintaining homeostasis despite external stresses. However, this balance breaks down with certain stress factors such as infection, anaemia, cold, heat, impatience and anger. Thus, the secretion of hormones from the brain or the adrenal gland is greatly related to fatigue.
Three factors (recovery in the supply of energy, rapid removal of fatigue substances, and stabilisation of hormone levels) are important in recovery from fatigue. Increasing the oxygen supply to a musculoskeletal system in the state of fatigue activates cellular activity, increases adenosine triphosphate (ATP) synthesis, and promotes the metabolism of fatigue substances. HBO can therefore be considered as a method of promoting recovery from fatigue.
Oxygen therapy should not be performed unnecessarily and superfluously because of its benefits in recovery promotion from fatigue. Increased levels of oxygen in the blood can cause tissue damage by oxidation. Therefore, it is necessary to maintain optimal oxygen balance by considering factors such as application times, concentration and pressure, which are developed from the understanding of the theoretical background of HBO.
2. Principles of Hyperbaric Oxygen (HBO) Treatment
Oxygen is usually taken into the blood from alveoli by breathing, where it combines with the haemoglobin in blood and is carried to peripheral tissues. However, since the oxygen absorption of haemoglobin is low at 100mm Hg, the oxygen saturation is limited by the haemoglobin concentration in the blood. By performing HBO treatments, ac- cording to Henry’s law (in the conditions of temperature regularity, the quantity of the gas dissolved in contact with a liquid is proportional to partial pressure of the gas), more oxygen is dissolved in the plasma of the pulmonary vein via the alveolar, which increases oxygen that reaches the peripheral tissues. Consequently, using pure oxygen with twice the atmospheric pressure, it becomes possible to raise the partial pressure of oxygen to near the 1000mm Hg. This is essentially the conditions of application of HBO for medical treatment.
In HBO treatment, the capacity of the gas stored inside the body is reduced by high pressure, and then the partial oxygen pressure (pO2) of arterial blood is raised in the treatment of diseases such as hypoxia disease, cell damage from infection, or a malignant tumour. Although these effects are the same for each disease, this treatment is currently used only in the field of emergency medicine. HBO treatment of an injury should:
• reduce swelling of soft tissue;
• promote the medical treatment of ligament damage or fracture;
• reduce the pain accompanying ischaemia;
• prevent infection (based on oxygen toxicity).
The relationship between wound recovery and oxygen supply deserves attention; basic research on this has prospered in recent years.
2.1 The Effect of HBO on Recovery Promotion of an Injury
The injured body part has a shortage of oxygen as a result of inhibited blood flow, swelling and a drop in capillary blood vessel permeability. The main focus of HBO treatment is to cancel the shortage of oxygen in a damaged body part. Kivisaari and Ni- inikoski[4] have reported measurement of pO2 in subcutaneous tissue in rats. The pO2 of injured tissue is generally about 5–15mm Hg, which is low compared with normal tissue (40–45mm Hg). Al- though the elevation of pO2 is expected to cause several effects on the damaged tissue, each were examined separately during recovery periods.
During the inflammatory phase of healing, HBO reduces the oedema, the swelling around the dam- aged part, and sharp pain. When Skyhar et al.[5] created the compartment syndrome (e.g. rise of muscle pressure of the anterior lower thigh part by oedema, swelling and crushing) of the dog leg, HBO of 2 atmospheres absolute (ATA) pure oxygen sub- sequently reduced muscular wet weight, and it is reported that mitigation of swelling was seen. However, in clinical research using human subjects, it seems that there is not such a large improvement. When Staple and Clement[6] performed HBO treatment on 66 people with muscular pain of the quadriceps femoris, the group that received the HBO treatment reported no large difference in recovery, especially regarding subjective sharp pain. Furthermore, when Borromeo et al.[7] performed the HBO treatment on 32 patients with acute leg joint sprains, they also reported that the mitigation of sharp pain and swelling did not occur appreciably. However, fur- ther research is needed to evaluate HBO due to the poor system for evaluating the effect on patients.
HBO treatment is expected to affect remodelling of damaged tissue, angiogenesis and synthetic production of extracellular matrix components (especially collagen etc.). Generally, it is supposed that vascular endothelial growth factors are stimulated, and the low oxygen stimulus in the convalescence of an injury works in the favour of blood vessel regeneration. However, according to the report of Mechine et al.,[8] treatment with HBO results in a rise of blood vessel density under granulation, and promotes a blood vessel bud. Whether HBO is advantageous over low oxygen therefore involves the consideration of many factors. Many effects in the regeneration of damaged tissue and angiogenesis have been reported. Kivisaari and Niinikoski[9] re- ported that intermittent HBO for 2 hours twice daily had no significant influence on the closure rate of open skin wounds with normal blood supply; how- ever, in ischaemic wounds, HBO enhanced the wound closure rate in the final healing stage. Moreover, according to Uhl et al.,[10] it is believed that the effects of the 100% oxygen twice daily HBO treatment (2 ATA/45 minutes) improves re-epithelisation in normal and ischaemic skin tissue.
The recovery process of a damaged medial col- lateral knee ligament has been investigated. Webster et al.[11] reported that the elasticity and fracture intensity of a ligament recovered to almost its nor- mal value within 4 weeks with HBO treatment (2.8 ATA/1.5 hours) and Mashitori et al.[12] also reported that type I procollagen gene expression at 7 or 14 days after injury was significantly higher in the HBO group and the ultimate load and stiffness was significantly greater at 14 days (2.5 ATA/2 hours). When Best et al.[13] examined the influence of the contraction ability of flounder-line damaged reproductive organs on rats, the HBO treatment (3 ATA) showed that the recovery effect may vary with different types of muscle fibres. When we looked at the influence of HBO on the repair of partial transection of the patella ligament in rats, more messenger RNA (mRNA) levels for type I procollagen were produced after HBO treatment. In 7–14 days after injury, mRNA levels for type I procollagen were found to be 1.4- to 1.5-fold greater in the HBO-treated group (2 ATA/60 minutes).[1,4] Furthermore, condi- tions of 2 ATA/60 minutes was compared with 2 ATM/30 minutes and 1.5 ATA/30 minutes using the same experiment model for 2 weeks. When collagen tissue was compared among the three groups that underwent the HBO treatment, the speed of liga- ment recovery occurred in the order of 2 ATA/60 minutes first, followed by 2 ATA/30 minutes, and finally 1.5 ATA/30 minutes.[14] Although these re- ports suggest that HBO is advantageous for medical treatment, the optimal conditions for treatment (atmospheric pressure, duration of sessions, frequency of session, and duration of treatment) still need to be determined. Furthermore, while injuries involving bones, muscles and ligaments have shown promising results, HBO treatment of cartilage tissue, which is generally in a low oxygen environment, might actually be detrimental.
Our previous research in sport injury involved 22 general athletes with various injuries including seven leg joint sprains, four knee ligament damages, four partial muscle ruptures, three peripheral nerve injuries, two fractures and two other injuries.[15] Depending on the clinical condition of the patient, atmospheric pressure was set between 1.3–2 ATA, and the exposure time was from 30 to 90 minutes. The evaluation of the patients afterwards included both subjective and objective symptoms. As a result, ≥70% of the patients experienced improvement (table I). Furthermore, there was a correlation between improvement and time from the injury in which the treatment was administered. Although there were

five ‘no change’ cases, there were no ‘worsening’ cases and adverse effects, other than slight ear pain, were not reported by any of the patients.
2.2 The Effect of HBO on Physical Conditioning
Factors that improve the conditioning of muscles and internal organs where transient oxygen is insufficient have recently been investigated. Fischer et al.[16] have reported that HBO treatment between games of tennis removes ammonia from the blood, leads to quicker recovery from fatigue, and prepares the player for the next game. In this study, conditions for the HBO treatment were milder than the conditions for medical emergencies. Also, atmospheric pressure does not need to exceed 1.5 ATA and the exposure time to oxygen is for no longer than 30 minutes. Haapaniemi et al.[17] twisted a tourniquet around the thigh of a rat and created a sparse blood model of the leg for the testing of
HBO. Compared with controls, 2.2 ATA for 45 minutes led to increases in ATP and phosphocreatine levels in muscle 4 hours later. Additionally, lower lactic acid levels were observed in these patients. The removal of lactic acid was eliminated more quickly with HBO treatment in six men 48 minutes after exercise. In subjects inhaling air for 45 minutes at 1 atmospheric pressure, lactic acid removal was 61.0%. In patients inhaling pure oxygen for 45 minutes at 1.0 ATA, removal was 64.7%; for 45 minutes at 1.3 ATA, removal was 76.0%; and for 45 minutes at 2.0 ATA, removal was 70.0% (figure 1). The setting atmospheric pressure performed with 1.3 ATA was significantly higher than that of others.[1,8] Therefore, HBO is not only expected to be beneficial for an externally caused injury, but also for improving training and conditioning for athletes. It is believed, however, that further re- search is necessary to develop optimised HBO guidelines tailored to each type of injury and conditioning.
The best experience of HBO use as a recovery method from muscular fatigue occurred during the Nagano Winter Olympics with seven participating athletes. After physical activity, the athletes received HBO treatment for 30–40 minutes at 1.3 ATA, with a maximum of six times per athlete and an average of two times per athlete. An athlete who experienced tension and sharp pain of the abdominal muscles was able to play a game after HBO treatment with almost no pain. Another player who was experiencing anterior knee pain was treated within 2 days of injury and was able to perform afterwards with no difficulty. These test cases show that HBO treatments demonstrate high performance without adverse effects such as muscular pain and nerve paralysis. Players were also able to benefit from the conditioning effects of HBO treatment.
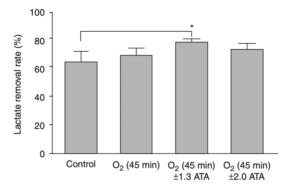
Fig. 1. Lactate removal rate under different conditions. The lactate removal rate = (the value of blood lactate at 3 min after exercise – the value of blood lactate at 48 min after exercise) × 100/the value of blood lactate at 3 min after exercise. Data are means ± SD, * p < 0.05 (vs control) [reproduced from Ishii et al.,[18] with permission]. ATA = atmospheres absolute.
3. Administration
So far, we have talked about the theoretical back- ground of HBO and basic research already done on HBO. The following sections now discuss the clinical application of HBO treatment.
3.1 Adverse Effects
As with all treatments, the adverse effects of HBO must be examined and determined to be less serious than the benefits of the treatment. HBO, by increasing oxygen levels, poses a risk to DNA through oxidative damage. The increased levels of oxygen increase oxygen radicals in cells, which are able to attack and degrade DNA. The detrimental action by such oxygen is called oxygen poisoning, the main target of which is the CNS and the lungs. As a clinical condition, the symptoms of oxygen poisoning include uneasiness in the front chest, nausea, vomiting, giddiness and tinnitus. Since these CNS symptoms tend to occur in the brain, they are generally called symptoms of brain oxygen poison- ing. For example, the congestion of an oedema in the alveolar, glass film formation and non-air alveolar are pathological changes that occur in the lungs. Although such symptoms have not occurred during HBO treatment, longer durations of treatment re- quire these possibilities to be taken into consideration.
We have studied the hormonal influence of HBO after ligament injury in adolescent rats. Forty male Wistar rats (aged 8 weeks) were used in this study. Prior to the experiment, the rats were housed in cages for 1 week. After 9 weeks of age, rats were anaesthetised and a wound creation was made in the
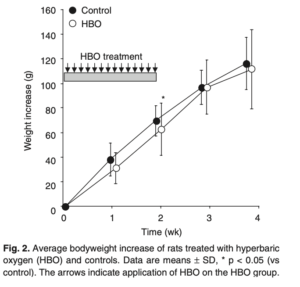
middle of the patellar ligament by the same method as our previous reports.[19] Rats were divided after wound creation into two groups (n = 20). In the HBO group, rats were treated with HBO at 2 ATA for 60 minutes/day (311.2 ± 17.2g), and in the control group, rats were merely exposed to air. In the HBO group, HBO was applied 14 times over the first 2 weeks. After 2 weeks, rats were without HBO. Rats were fed a standard diet and housed in individual cages. As a result, whole bodyweight increased with time in both the HBO and the control groups. After 2 weeks of HBO treatment, the aver- age weight increase of the HBO rats was significantly less than that of the control group (p < 0.05) [figure 2]. However, there were no significant differences in weight increase between the two groups at 1, 3 and 4 weeks. Values of plasma growth hormone (GH) and plasma thyroid stimulating hormone (TSH) are shown in figure 3. There were no significant differences in plasma GH or plasma TSH between the HBO group and the control group at 1 and 2 weeks. These results suggest that HBO has influenced the whole bodyweight in the adolescent rats during HBO application, However, this was a temporary response and did not influence plasma hormone level in the blood. Further studies are needed, but it appears we have to take care with the use of HBO for young athletes.
3.2 Safety Control
Before HBO treatment can find widespread use in the sports field, it would require the standardisation of equipment and safety regulations. Physicians would need to be trained by engineers about the safety standards of hyperbaric environmental medicine. The medical community would become responsible for such systems, but explosions have occurred five times previously in Japan, which has

caused resistance to HBO treatment. Although a system that compresses air rather than pure oxygen would be likely to be safer, such a system would most likely not achieve the same medical effects. Additionally, safety standards must be such that the risk of an explosion is almost zero, not such that the risk is simply reduced through the use of com- pressed air.
With further research it should be possible to tailor treatment to an individual’s condition and issue an exact diagnosis and medical treatment plan. Although it seems that the price of each treatment of HBO costs several hundred dollars in the US, in Japan we cannot carry out HBO treatment using health insurance payment for sports injuries, and private payment is needed. Therefore, before using HBO treatment, it will be necessary to explain the costs and limitations to the individual players and the team medical staff beforehand, and also to make it clear that it is only to be used complementary to other treatments.
4. Conclusions
HBO treatment has been shown to be promising for tissue remodelling after injury and for the recovery of fatigue. However, further research is required, focusing on tailoring treatment to an individual’s condition, which will allow efficient use of HBO.
Acknowledgements
All authors agree with the contents of the manuscript and affirm that this work has not been submitted or published elsewhere. The authors would like to acknowledge Prof. Tetsuya Tateishi of the National Institute for Materials Sciences and Prof. Takashi Ushida of the University of Tokyo. The authors would also like to thank Dr Tsukasa Kanda and Dr Takeo Imada for their valuable assistance in these research projects. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Jain K. Textbook of hyperbaric medicine. 3rd ed. Germany: Hogrefe & Huber Publisher, 1999
2. Boerema I, Meyne NG, Brummelkamp WK, et al. Life without blood. J Cardiovasc Surg (Torino) 1960; 1: 133-46
3. James PB, Scott B, Allen MW. Hyperbaric oxygen therapy in sports injuries. Physiotherapy 1983; 79: 571-2
4. Kivisaari J, Niinikoski J. Use of silastic tube and capillary sampling technique in the measurement of tissue PO2 and PCO2. Am J Surg 1973; 125: 623-7
5. Skyhar MJ, Hargens AR, Strauss MB, et al. Hyperbaric oxygen reduces edema and necrosis of skeletal muscle in compartment syndromes associated with hemorrhagic hypotension. J Bone Joint Surg 1986; 68-A: 1218-24
6. Staple J, Clement D. Hyperbaric oxygen chambers and the treatment of sports injuries. Sport Med 1996; 22: 219-27
7. Borromeo CN, Ryan JL, Marchetto PA, et al. Hyperbaric oxygen therapy for acute ankle sprains. Am J Sports Med 1997; 25: 619-25
8. Mechine A, Rohr S, Toti F, et al. Wound healing and hyperbaric oxygen: experimental study of the angiogenesis phase in the rat [in French]. Ann Cir 1999; 53: 307-17
9. Kivisaari J, Niinikoski J. Effects of hyperbaric oxygenation and prolonged hypoxia on the healing of open wounds. Acta Chir Scand 1975; 141: 14-9
10. Uhl E, Sirsjo A, Haapaniemi T, et al. Hyperbaric oxygen improves wound healing in normal and ischemic skin tissue. Plast Reconstr Surg 1994; 93: 835-41
11. Webster DA, Horn P, Amin HM, et al. Effect of hyperbaric oxygen on ligament healing in a rat model. Undersea Hyperb Med 1996; 23 Suppl.: 13
- Mashitori H, Sakai H, Koibuchi N, et al. Effect of hyperbaric oxygen on the ligament healing prodcess in rats. Clin Orthop 2004; 423: 268-74
- Best TM, Loitz-Ramage B, Corr DT, et al. Hyperbaric oxygen in the treatment of acute muscle stretch injuries: results in an animal model. Am J Sports Med 1998; 26: 367-72
- Ishii Y, Ushida T, Tateishi T, et al. Effects of different exposure of hyperbaric oxygen on ligament healing in rats. J Orthop Res 2002; 20: 70-3
- Ishii Y, Miyanaga Y, Shimojo H, et al. The role of hyperbaric oxygen for the early return to sports activities [in Japanese]. J Musculoskeletal Syst 1999; 12: 785-9
- Fischer B, Lehrl S, Jain K, et al. Handbook of oxygen therapy. Berlin: Springer Verlag, 1988: 251-26
- Haapaniemi T, Sirsjo A, Nylander G, et al. Hyperbaric oxygen treatment attenuates glutathione depletion and improves meta bolic restitution in post -ischemic skeletal muscle. Free Radic Res 1995; 23: 91-101
- Ishii Y, Miyanaga Y, Shimojo H, et al. The effect of hyperbaric oxygen therapy on lactate concentration after maximal exer- cise [in Japanese]. Jpn J Hyperbaric Med 1995; 30: 109-14
- Ishii Y, Miyanaga Y, Shimojo H, et al. Effects of hyperbaric oxygen on procollagen messenger RNA levels and collagen synthesis in the healing of rat tendon laceration. Tissue Eng 1999; 5: 279-86
Correspondence and offprints: Dr Yoshimasa Ishii, Depart- ment of Orthopaedic Surgery, Hiroshima University, 1-2-3, Kasumi, Minamiku, Hiroshima, 734-0022, Japan.
E-mail: yoishii@hiroshima-u.ac.jp



